29/04/15
27/04/15
Bile Esculin Agar
Bile Esculin Agar (BEA) is a selective differential agar used to isolate and identify members of the genus Enterococcus, also known as "group D streptococci".
Bile esculin agar contains oxgall (bile salts) to inhibit the growth of gram positive organisms other than enterococci and group D streptococci. It also contains nutrients, esculin, and ferric citrate. When an organism hydrolyzes the glycoside esculin to form esculetin and dextrose, the esculetin reacts with the ferric citrate to produce a dark brown or black phenolic iron complex.
If an organism can hydrolyze esculin, the media will turn dark brown or black. However, the test is interpreted as a positive result only if more than half the medium is dark brown or black after incubation.
Bile-esculin agar medium is prepared as agar slants or plates.
The constituent of Bile-esculin agar medium are:
- Peptone
- Beef extract
- Oxgall (Bile)
- Esculin
- Ferric citrate
- Agar
Bile esculin medium contains esculin and peptone for nutrition and bile to inhibit Gram-positive bacteria other than Group D streptococci and enterococci. Ferric citrate is added as a color indicator.
Principle: Bile-esculin test is based on the ability of certain bacteria, notably the group D streptococci and Enterococcus species, to hydrolyze esculin in the presence of bile (4% bile salts or 40% bile).
Note: Many bacteria can hydrolyze esculin, but few can do so in the presence of bile
Case Files Biochemistry
Often, the medical student will cringe at the “drudgery” of the basic science courses and see little connection between a field such as biochemistry and clinical problems. Clinicians, however, often wish they knew more about the basic sciences, because it is through the science that we can begin to understand the complexities of the human body and thus have rational methods of diagnosis and treatment.
This book is organized for versatility: to allow the student “in a rush” to go quickly through the scenarios and check the corresponding answers and to provide more detailed information for the student who wants thought-provoking explanations. The answers are arranged from simple to complex: a summary of the pertinent points, the bare answers, a clinical correlation, an approach to the biochemistry topic, a comprehension test at the end to reinforcement or emphasis, and a list of references for further reading. The clinical cases are arranged by system to better reflect the organization within the basic science.
Finally, to encourage thinking about mechanisms and relationships, we intentionally did not primarily use a multiple-choice format. Nevertheless, several multiple-choice questions are included at the end of each scenario to reinforce concepts or introduce related topics.
Finally, to encourage thinking about mechanisms and relationships, we intentionally did not primarily use a multiple-choice format. Nevertheless, several multiple-choice questions are included at the end of each scenario to reinforce concepts or introduce related topics.
You can download this book at HERE
26/04/15
Contoh KRS AAK Nasional Surakarta
Berikut ini adalah contoh KRS(Kartu Rencana Studi) AAK Nasional Surakarta
Untuk gambar yang lebih jelas silahkan kunjungi link DI SINI
16/04/15
Microbiology Of Food
Food
is an indispensable item for all living organisms. All food items are
associated with microorganisms in one form or other. Foods get contaminated
during handling, harvest, transport and storage. Foods also get contaminated
due to the methods of food collection, cooking and preparation. Food forms an
ideal culture medium for the growth and multiplication of microorganisms.
15/04/15
Sterilization
Sterilization is the freeing of an article from all living
organisms, including bacteria and their spores. Sterilization of culture media,
containers and instruments is essential in microbiological work for isolation
and maintenance of microbes. In surgery and medicine, the sterilization of
instruments, drugs and other supplies is important for the prevention of
infection.
Sterilization can be effected in a variety of ways, which can be
conveniently categorized as follows:
1.
Physical methods
a.
Heat
Dry heat
Mechanism of killing
by dry heat:
Dry heat kills the
organisms by destructive oxidation of essential cell constituents
Killing of the most
resistant spores by dry heat requires a temperature of about 160 °C for 60
minutes
Dry heat is employed
for glassware; syringes, metal instruments and paper wrapped goods, which are
not spoiled by high temperatures
l It is also used for anhydrous fats, oils and powders that are
impermeable to moisture
METHODS OF
STERILIZATION BY DRY HEAT:
1. RED HEAT
Inoculating wires, points of forceps and searing spatulas are sterilized
by holding them in the flame of Bunsen burner until they are seen to be
red-hot.
2. FLAMING
This method is used for sterilizing scalpel, mouth of culture tubes,
glass slides etc.
It involves passing of an article through Bunsen flame without allowing
it to become red-hot.
3. HOT AIR OVEN
This is the main means of sterilization by dry heat. Exposure at a
temperature of 160 °C for 1 hour is generally employed.
4. INFRARED RADIATIONS
Source employed is an electrically heated element, the infra red
rays are directed on to the object to be sterilized and temperature of 180 °C
can be obtained.
Moist heat
Mechanism of killing
by moist heat:
Moist heat kills the organisms by coagulating and denaturing their
enzymes and structural protein
Sterilization by moist
heat of the most resistant spores generally requires 121 °C for 15-30 minutes
Moist heat is used for
the sterilization of culture media, and all other materials through which steam
can penetrate
Moist heat is more
effective than dry heat
Sterilization can be
done at lower temperatures in a given time at a shorter duration at the same
temperature
METHODS OF
STERILIZATION BY MOIST HEAT
Moist heat can be employed at
1. Temperature below 100 °C
Examples : pasteurization
of milk
In Pasteurization of
milk the temperature employed is either 63 °C for 30 minutes or 72 °C for 20
seconds. All nonspore-forming pathogens in milk like Salmonellae,
M.tuberculosis are killed.
2. Temperature of 100
°C
3. Temperature above 100 °C
Examples : Sterilization
in an autoclave
Autoclaving is the
most reliable method
It is the method most widely used for sterilization of culture media
and surgical supplies
When water is boiled
within a closed vessel at an increased pressure, the temperature at which it
boils and the steam it forms will rise above 100 °C
This principle is used
in the autoclave
Normally autoclaving
is done at 15 lbs. (pounds per sq. Inch pressure) and 115 °C for 15 minutes
b.
Radiations
Ultraviolet radiations
Ionizing radiations
c.
Filtration
When fluids are passed
through bacteria stopping filters, they are made free from bacteria. l It is
useful for making preparations of soluble products of bacterial growth such as
toxins. Liquids that would be damaged by heat such as serum and antibiotic
solutions can be sterilized by filtration. Efficient filters should be able to
retain Serratia marcescens.
2.
Chemical methods
FACTORS INFLUENZING
STERILIZATION BY HEAT
a. The temperature and time: they are inversely related, shorter time
is sufficient at high temperatures.
b. Number of microorganisms and spores: The number of survivors diminished
exponentially with the duration of heating
c. Depends on the species, strains and spore forming ability of the
microbes.
d. Thermal death point is the lowest temperature to give complete killing
in aqueous suspension within 10 minutes
e. Depends on the nature of material: a high content of organic substances
generally tends to protect spores and vegetative organisms against heat.
f. Presence of organic or inorganic disinfectants facilitates killing
by heat
g. pH also plays an important role in the killing of microorganisms
TYPES OF FILTERS
There are different kinds of filters:
1. Earthenware candles - called Berkfield & Chamberland
filters
Berkfield Filters
Made from Kieselguhr, a fossil diatomaceous earth
Three grades of porosity are available:
a. Veil - coarsest one
b. N - normal one
c. W- wenig the finest one
Chamberland Filters
Made from unglazed porcelain
Four grades are available:
a. L1- clarifying filters
b. L1a-Big
c. L2 - normal
d. L3- Finest
2. Asbestos and asbestos-paper discs filters - called Seitz
filters
Made up of asbestos pads
Three grades are available:
a.
K- clarifying filters
b.
Normal
c.
Special EK bacteria stopping filters
3. Sintered glass filters
Made from sintered glass
Different grades available:
a.
Grades 1 to 5
b.
Grades 1-2 are for clarifying purpose
c.
Grades3-5 is for sterilization purpose
3.
Cellulose membrane filters
Made up of nitro-cellulose membranes. Made with
different grades of porosity by adjusting the concentration of constituents
4.
Fibre glass filters.
MERITS AND DEMERITS OF HEAT STERILIZATION
Advantages of heat sterilization:
1. Sterilization is very effective
2. Instruments are standardized to deliver the required effective
heat
3. Heat deliver system can be monitored effectively with various
controls like pressure gauge, temperature meters etc
4. Established quality control methods available
Disadvantages of heat sterilization:
1. Steam impermeable materials like fats, oils and powders can not
be sterilized by autoclaving.
2. Heat sensitive materials can not be sterilized by heat
Examples:
1. Serum can not be sterilized
2. Antibiotics
3. Plastic materials
4. Vaccines
5. Rubbers
3. Presence of organic matters interfere with effective
sterilization
4. Dangers of explosion when high pressure is used
14/04/15
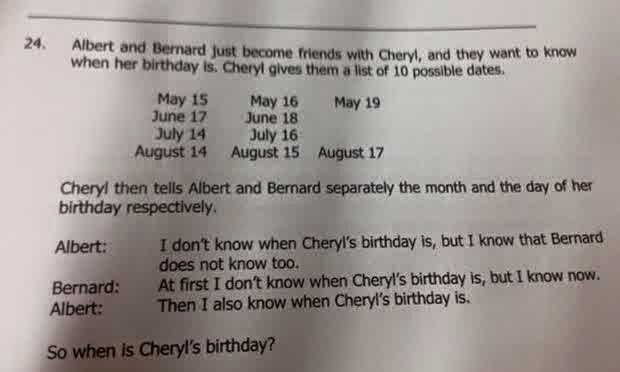
Singapore high school maths problem stumps the Internet
A maths problem that first appeared in a test for Singapore's elite high school students has baffled Internet users around the world after it went viral, prompting a rush of attempts to solve it.
The question, involving a girl asking two boys to guess her birthday after giving them scant clues, first appeared in an April 8 test organised by the Singapore and Asian School Math Olympiads (SASMO).
It was meant for 15- and 16-year-old elite secondary school students, but swiftly went global after a local television news presenter posted it on his Facebook page Saturday.
In the question, Cheryl gives her new friends Albert and Bernard 10 possible dates when they enquired about her birthday, before separately giving each of them further clues.
Test-takers are then asked to use logic to deduce Cheryl's birthday using a short conversation between the two boys about the information given to them.
By Monday Internet users around the world were posting meticulously detailed answers to the puzzle on social media networks such as Facebook and Reddit, only to prompt a slew of comments disputing their findings and methodology.
Others posted sardonic comments about "Coy Cheryl".
"Cheryl obviously didn't want Albert and Bernard at her party. Should have taken the hint when Cheryl decided to play this little game," wrote David Leong on Facebook.
The hashtag #cherylsbirthday also trended on Twitter, while some people created funny memes about the puzzle. "If Math would grow up and solve its own problems, that'd be great," read one such meme.
The "mind-boggling" problem also made the mainstream media, with leading websites including the Guardian newspaper and Buzzfeed publishing articles about the puzzle.
- Model answer -
In a Facebook post late Monday, SASMO provided the full question and a model answer, which can be found at https://www.facebook.com/4sasmo/posts/983396811695295
The post also clarified earlier erroneous reports that the question was not posed to primary school children, saying SASMO thought it important to specify the age of the students involved so "Singapore parents will not start to worry so much".
The question was "actually from the secondary 3 and secondary 4 SASMO contests held on April 8, 2015", it said, adding it was "meant to sift out the better students".
Following relentless but mostly friendly online debate about the question's difficulty level, SASMO's executive director Henry Ong on Tuesday afternoon issued another statement.
"We are pleased that this problem has generated so much interest and thinking from the public," Ong said.
"We are not saying this problem is for every student... but if this kind of problem can be used to stretch the better students to sharpen their analytical power, why not?"
Singapore is renowned worldwide for its national maths system, which has been emulated by schools in other developed countries and cities, including New York.
Singaporean pupils are ranked second in the world in mathematics according to the latest student assessment survey by the Organisation for Economic Cooperation and Development, beaten only by their counterparts in Shanghai.
Can you do it? Are you smarter than a Singaporean ten-year-old?
Go on, give it a try.
Advice For Dog Owners (Toxocara canis)
During recent years there has been much publicity about Toxocara canis and the risks, real and imagined, associated with this parasite. Whilst the problem should not be exaggerated, it is necessary for dog owners and the public generally to know what they should do to minimise the risk.
WHAT IS IT?
Toxocara canis is a parasite that lives inside dogs’ bodies. It is a round, white worm (looks like spaghetti) and it infects, most frequently, pregnant nursing bitches and young puppies. Infection can be passed on via the mother’s milk and dog’s droppings.
LIFE CYCLE
Pregnancy activates worm larvae which may be lying dormant in the bitch. Some will migrate to the womb, others to the mammary glands and into developing puppies. Other larvae will continue their lives in the intestine of the bitch. By the time the puppy is a fortnight old, larvae already within it will have developed into adult worms. The puppy will receive even more larvae from the bitch’s milk and from being licked by her. At the same time, the bitch will be reinfected when she cleans up her puppies droppings. Toxocara eggs hatch in the puppy and the larvae burrow from the gut and migrate via the liver to the lungs where they may cause respiratory problems. Some larvae spread via the blood to other tissues where they stay dormant. Some are coughed up, swallowed and mature into adult worms in the digestive system. These lay thousands of eggs which are passed out with the droppings, to lie on grass, plants and soil, sometimes for many months, until ingested again by another dog to start the whole cycle of infection again.
HOW TO RECOGNISE WORM INFESTATION IN YOUR DOG
Whether you see worms or not, it can be assumed that all unwormed puppies and nursing bitches carry worms. Heavy infestation in puppies can cause breathing problems and even pneumonia. Puppies will also show signs of abdominal pain, may whine and adopt a characteristic straddle leg position. Infested puppies suffer retarded growth, harsh coat and have a poor, pot bellied appearance when the stomach and intestine is full of worms. In extreme cases the digestive system may become blocked. It is strongly recommended that you regularly worm your pregnant bitch and the puppies with a preparation available from your vet and follow his advice on administering times.
THE RISK TO HUMANS
The eggs of toxocara canis are invisible to the naked eye but are sticky and may be picked up from soil, grass or the animal’s coat/bedding and may be swallowed later.
Eggs which are swallowed can hatch into larvae in humans but will not develop into adult worms. However, these tiny larvae will travel around the body – usually causing no problems. Very rarely though, they can settle in particularly sensitive tissue such as the retina of the eye, where they may cause damage or even blindness. Each year about 50 cases involving eye damage are recorded. Although this number is small, the effects upon individuals are traumatic and it is prudent to take precautions. Freshly passed dog droppings are not a direct hazard because the toxocara eggs need about three weeks to mature outside the dog before they become infective. So, whilst contact with droppings is unpleasant, it does not present a risk from this point of view however, mature eggs can remain viable in the ground for some time. This is why children are more at risk (through sports fields and playing in the park - rolling on the ground) and must wash hands and faces thoroughly after playing.
WHAT TO DO
• Worm your dog properly both as a puppy and as an adult. Consult your vet for advice on the most effective wormer, as some products brought over the counter can be less effective.
• It is vital to worm the bitch as well as her puppies (seek advice from your vet)
• Do not discontinue worming because you see no worms passed. Remember dogs can become reinfected.
• When you have carried out a worming for an infestation or if you see worms in the droppings, be sure to pick up and properly dispose of it. It should be burnt or flushed down the w.c rather than buried or composted.
• Keep kennels and sleeping areas clean.
• Try and prevent your dog fouling grassed areas used by the public. If it does, clean it up immediately with a poop scoop or bag and dispose of in a “dog bin”.
• Do not allow dogs to eat off crockery used by humans.
• Do not allow dogs to lick children’s faces or share food such as ice cream and biscuits.
• Always wash your hands (and face if necessary) after handling a dog, particularly a puppy or nursing bitch.
• Ensure that children always wash their hands and face after handling a dog, puppy or nursing bitch or after they have been playing on grassed areas. Following these simple straightforward precautions will protect the health of your dog, yourself and your family as well as the general public.
Microbiology Of Milk
Milk is the
white, fresh clean lateral secretion obtained from female cattle. Milk is used
for the nourishment of their younger ones. It is in liquid form without having
any colostrum. The milk contains water, fat, protein and lactose. About 80-85%
of the proteins is casein protein. Due to moderate pH (6.6), good quality of
nutrients, high water contents etc. make milk an excellent nutrient for the
microbial growth. It is mainly the udder interior, teats surrounding
environment and manual milking process make the source of contamination.
Sources
of microorganisms in milk
Milk secreted
into the udder is sterile. The first few strippings of milk contain more amount
of bacteria and the population of bacteria gradually decreases. It is observed
that last strippings of milk from the udder seems to be free from bacteria.
This clearly indicates that most of the microorganisms found in the milk are
from external source. The different sources of microorganism in milk are from:
1) The
udder of the cow
The milk producing animals should be kept
neat and clean. More care should be taken to keep the flanks, udder and teats
clean. The interior of the teats of the udder is warm and contains the last
remains of the milk which has more microbes which would have entered through
opening of teat and multiplied.
2) skin
of the cow
Soil, faeces and dirt adhere to the skin and hairs
of the cow. Hair, dirt and dust fall in to milking utensils or into the teat
cups of milking machines. Most of the organisms from these 109 110 sources are
gas producers and putrefactive types. Faeces contain enormous quantity of
organisms and most of them are pathogenic microorganisms.
3) utensils
and equipment
Milking utensils and equipments are the major
sources of contamination of milk. They have to be washed properly with
detergent. Further the utensils and equipments should be cleaned with hot
water, air and steam to remove all the spore forming, fluorescent and coliform
microorganisms.
4) feeds
Microorganisms are found everywhere. They are
present in abundant in vegetation and soil. Dry feeds have more amount of
bacteria and less amount of fungi. These organisms contaminate the milk.
5) air
of the cow shed
The air of the cow shed is greatly contaminated
by dry dirt and dust. During the mixing of feeds and during the cleaning
process of the floor, the air of the cow shed is highly contaminated and it is
passed on to the milk.
6) milking
persons
Pathogenic microorganisms may enter into the
milk through milking persons. They should wear clean clothes and properly wash
their hands before milking. Nails should be cleaned and trimmed. Discharge from
sneezing, coughing and nose blowing should not reach the atmosphere, equipment
or the milk. Some of the organisms may be carriers of diseases.
7) water
Pure water should be used for cleaning
purposes. Water exposed to contamination spreads the microorganisms. Water should
be free from coliform organisms. Chlorination of water prevents such
contamination.
:
Microbiological
standard and grading of milk
The Indian
Standard Institute (ISI) has prescribed microbiological standard for quality of
milk.
1. Coliform
count in raw milk is satisfactory
if coliforms are absent in 1:100 dilution.
2. Coliform
count in pasteurized milk is satisfactory if coliforms are absent in 1:10
dilution.
Microbiological
quality of milk
Grading
of milk
The quality of
milk is judged by certain standards and it is known as grading milk. Grading of
milk is based upon regulations pertaining to production, processing and
distribution. This includes sanitation pasteurization holding conditions and
microbiological standards. The U.S Public Health Secrine Publication ‘Milk
Ordinance and code’ shows the following chemical, bacteriological and
temperature standards for grade A milk and milk products.
13/04/15
Gram's Staining
The Gram staining method is named after the Danish bacteriologist Hans Christian Gram (1853 – 1938) who originally devised it in 1882 (but published in 1884), to discriminate between pneumococci and Klebsiella pneumoniae bacteria in lung tissue. It is a differential staining method of differentiating bacterial species into two large groups (Gram-positive and Gram-negative) based on the chemical and physical properties of their cell walls. This reaction divides the eubacteria into two fundamental groups according to their stainability and is one of the basic foundations on which bacterial identification is built. Gram staining is not used to classify archaea, since these microorganisms give very variable responses.
Gram staining consists of four components:
• Primary stain (Crystal violet, methyl violet or Gentian violet)
• Mordant (Gram's Iodine)
• Decolourizer (ethyl alcohol, acetone or 1:1 ethanol-acetone mixture)
• Counterstain (Dilute carbol fuchsin, safranin or neutral red)
The original description of staining technique by Christian Gram in a publication titled "The differential staining of Schizomycetes in tissue sections and in dried preparations" in Fortschitte der Medicin; 1884, Vol. 2, pages 185-189 was slightly different from what we use today. The primary stain used was aniline gentian violet, mordant was Lugol's iodine (iodine-potassium iodide in water), decolorizer was absolute alcohol and bismark brown was the counterstain.
Procedure:
The smear on a glass slide is covered with few drops of one of the primary stains. Gentian violet is a mixture of methyl violet and crystal violet. The primary stain renders all the bacteria uniformly violet. After a minute of exposure to the staining solution, the slide is washed in water.
The smear is treated with few drop of Gram's Iodine and allowed to act for a minute. This results in formation of a dye-iodine complex in the cytoplasm. Gram's iodine serves as a mordant.
The slide is again washed in water and then decolorized in absolute ethyl alcohol or acetone. A mixture of ecetone-ethyl alcohol (1:1) can also be used for decolorization. The process of decolorization is fairly quick and should not exceed 30 seconds for thin smears. Acetone is a potent decolorizer and when used alone can decolorize the smear in 2-3 seconds. A mixture of ethanol and acetone acts more slowly than pure acetone. Decolorization is the most crucial part of Gram staining and errors can occur here. Prolonged decolorization can lead to over-decolorized smear and a very short decolorization period may lead to under-decolorized smear.
After the smear is decolorized, it is washed in water without any delay. The smear is finally treated with few drops of counterstain such as dilute carbol fuchsin, neutral red or safranin.
The slide is washed in water; excess water is removed using a blotting paper, dried in air and heat fixed before observing under microscope.
Those bacteria that hold on to primary dyeiodine complex and remain violet are called
Gram positive and those which get decolorized and subsequently take up counterstain (pink/red) are called Gram negative.
Basic fuchsin (present in dilute carbol fuchsin) stains many Gram negative bacteria more intensely than does safranin, making them easier to see. Some bacteria which are poorly stained by safranin, such as Haemophilus spp., Legionella spp., and some anaerobic bacteria, are readily stained by basic fuchsin.
In order to ascertain if the staining procedure was satisfactorily conducted, a control smear of known Gram positive organism (e.g.,Staphylococcus aureus) and a known gram
negative organism (Escherichia coli) must be stained simultaneously. While the fibrin in a clinical specimen may appear gram positive, the pus cells and epithelial cells are always gram negative.
Mechanism of Gram reaction:
Various theories have been proposed to explain why some bacteria retain the dye and
some don't. Theories such as differences in cytoplasmic pH (2 in case of Gram positive
bacteria and 3 in case of Gram negative bacteria), and presence of Magnesium ribonucleate in Gram positive bacteria and its absence in Gram negative bacteria have not received widespread acceptance. The thickness of Gram positive cell wall and
presence of more lipids in Gram negative cell walls have been more acceptable reasons for Gram stain reactions. It is believed that the positively charged crystal violet pass through the cell wall and cell membrane and binds to negatively charged components inside the cell. Addition of negatively charged iodine (in the mordant) binds to the positively charged dye and forms a large dye-iodine complex within the cell. Crystal violet (hexamethyl-para-rosaniline 3 chloride) interacts with aqueous KI-I2 via a simple anion exchange to produce a chemical precipitate. The small chloride anion is replaced by the bulkier iodide, and the complex thus formed becomes insoluble in water. During decolorization, alcohol dissolves the lipid present in the outer membrane of Gram negative bacteria and it leaches the dye-iodine complex out of the cell. A thin layer of peptidoglycan does not offer much resistance either. The dye-iodine complexes are washed from the Gram negative cell along with the outer membrane. Hence Gram
negative cells readily get decolorized. On the other hand Gram positive cells become dehydrated from the ethanol treatment, closing the pores as the cell wall shrinks during dehydration. The dyeiodine complex gets trapped inside the thick peptidoglycan layer and does not get decolorized.
Limitations of Gram staining:
Some Gram-positive bacteria may lose the stain easily and therefore appear as a mixture of Gram-positive and Gram-negative bacteria (Gram-variable). When over-decolorized, even Gram positive bacteria may appear pink and when under-decolorized gram negative bacteria may appear Gram positive.
The Gram reaction also depends on the age of the cell. Old cultures of Gram positive bacteria (where cell walls may be weakened) may readily get decolorized. Gram positive cells affected by cell wall active agents such as lysozyme or antibiotics may become Gram negative. Gram-positive bacteria such Actinomyces, Arthobacter, Corynebacterium, Mycobacterium, and Propionibacterium have cell walls particularly sensitive to breakage during cell division, resulting in Gram-negative staining of these cells. In cultures of Bacillus, and Clostridium a decrease in peptidoglycan thickness during cell growth may cause some of them to appear Gram negative.
Certain group of bacteria can display variable response to the stain, which can be due to growth stress (e.g., unsuitable nutrients, temperatures, pHs, or electrolytes) that results in a number of nonviable, gram-negative cells in a gram positive culture, but certain bacterial species are known for their gram variability even under optimal growth conditions. Some bacteria tend to appear Gram negative when grown in acidic medium. Loss of cell walls in Gram positive bacteria may render them Gram negative (L-forms). Bacteria totally devoid of cell wall (Mycoplasma) are always Gram negative. Bacteria such as Mycobacterium that have extra waxy content in their cell wall are difficult to stain. Small and slender bacteria such as Treponema, Chlamydia, Rickettsia are often difficult to stain by Gram's method. Gram positive bacteria that have been phagocytosed by polymorphs may also appear Gram negative.
Modifications of Gram stain:
There have been several modifications of Gram's stain. These are:
1. Kopeloff and Beerman's modification: Primary stain solution consists of freshly
constituted methyl violet with sodium bicarbonate in distilled water. Mordant consists of iodine dissolved in 4% NaOH solution. Decolorization is either using acetone alone or a mixture of acetone and ethanol. Basic fuchsin is used to counterstain the smear. This method may be modified to stain tissue sections.
2. Jensen's modification: This method involves use to methyl violet as primary stain,
iodine and potassium iodide in water as mordant, absolute alcohol as decolorizer and neutral red as counterstain. For Neisseria spp, Sandiford's counterstain is useful.
3. Weigert's modification: This modification is particularly useful for staining tissue
sections. The primary stain carbol gentian violet is prepared using saturate alcoholic solution of 4gentian violet and 5% phenol solution. Gram's iodine is used as a mordant and aniline-xylol is used as a decolorizer. The counterstain carmalum (carminic acid and potassium alum in water), however is used ahead of primary stain. This method may be used to stain Pneumocystis cysts.
4) Preston and Morrell's modification: The primary stain used in this modification is
ammonium oxalate-crystal violet. The smear is washed in Lugol's iodine and further treated with iodine solution. The smear is decolorized using iodine-acetone decolorizer and counterstained using dilute carbol fuchsin solution. This method has been further modified to overcome the irritating iodine in aerosols by reducing the iodine concentration to one-tenth and shortening the duration of decolorization to ten seconds.
Applications of Gram staining:
1) Differentiation of bacteria into Gram positive and Gram negative is the first step towards classification of bacteria.
2) It also the first step towards identification of bacteria in cultures.
3) Observation of bacteria in clinical specimens provides a vital clue in the diagnosis of
infectious diseases.
4) Useful in estimation of total count of bacteria.
5) Empirical choice of antibiotics can be made on the basis of Gram stain’s report.
6) Choice of culture media for inoculation can be made empirically based on Gram’s stain report.
Miscellanea:
• Although Gram stain is useful in staining bacteria, certain fungi such as Candida and
Cryptococcus are observed as Gram positive yeasts.
• Half-Gram stain refers to modified staining technique, where the smear is neither
decolorized nor counterstained. It is useful to stain a known Gram positive bacterium.
• Rapid Gram stain refers to quickened technique where the smear is exposed to only 30 seconds instead of one minute.
• In specimen such as sputum, capsulated bacteria may stand out as clear spaces between the bacterium and the pink (mucus) background.
• The spores may stand out as clear, unstained region in sporing bacteria.
microrao.com
Langganan:
Komentar (Atom)